Parenting
0 min read
RSV in babies: Why this common virus can turn serious in newborns

Medically Reviewed Dr. Steven Goldberg, MD, MBA, Chief Medical Officer at HealthTrackRx. And, Jose Luis Salas, Infection Prevention & Control Director at El Paso Children’s Hospital.
Written by Cradlewise Staff
It’s that time of the year again, when sniffles, leaky noses, and tiny coughs make a comeback. And if you’re a parent to a newborn or young baby, you probably already know the mix of dread and hyper-vigilance that comes with it.
Every sneeze feels like a mini alarm, every stuffy nose makes you wonder if it’s just a cold or something more serious. Because while most seasonal sniffles are harmless, one virus in particular, RSV (Respiratory Syncytial Virus), can turn a regular cold into a worrisome situation, especially for newborns. It spreads fast, hits hard, and can sometimes sneak its way into the lungs, causing breathing trouble in babies who are still learning to take on the world one tiny breath at a time.
Here’s the thing: RSV is common (in fact, according to the CDC, nearly every child will have it by age 2 in many parts of the world). But for newborns and very young babies? It can sneak up and become a serious issue. Before we dive in, we spoke with Dr. Steven Goldberg, MD, MBA, Chief Medical Officer at HealthTrackRx, and Jose Luis Salas, Infection Prevention & Control Director at El Paso Children’s HospitalTexas. They walk us through what RSV is, why it’s so common, and when it can actually become serious in little ones.
To understand just how common RSV is in the U.S., Dr. Steven Goldberg shares: “RSV is the leading cause of lower respiratory tract infection (LRTI) and hospitalization among infants in the United States. The annual incidence in infants under 12 months is approximately 592,700 cases.” He adds that even infants with no risk factors can experience severe illness.
Signs of RSV in babies
When we talk about “signs,” we mean the things you can see, such as how your baby is breathing, feeding, and responding. Since babies can’t tell us when something feels off, they show it in small ways, and it’s often up to us to notice those little changes.
Here are some signs to keep an eagle eye on:
- Runny nose or congestion. While this could just be a mild cold, in a baby, that’s our first flag.
- Eating or drinking less than usual, fewer wet nappies. In very young infants (especially under 6 months), this is a big sign.
- Faster breathing than usual, or the kind of “working harder” to breathe: you might see the sides of the ribs pulling in, flaring of nostrils, “belly breathing” or the baby’s head bobbing when they breathe.
- Wheezing or a higher-pitched cough, or grunting during breaths. That’s the sign the lower airways might be involved.
- In very young infants: irritability, decreased activity (baby seems “off”), or, alarmingly, apnea (pauses in breathing for 10+ seconds) in babies less than 6 months.
To help parents understand when RSV is moving deeper into the lungs, Jose Luis Salas, explains: “When RSV starts to move deeper into the lungs, the breathing changes. You might notice faster breathing, ribs pulling in, nostrils flaring, wheezing, or feeding difficulties.”
When to call the pediatrician?
Because RSV can get worse quickly in some babies, it’s important to know when to call the doctor right away. According to the American Academy of Pediatrics, you should reach out if you notice:
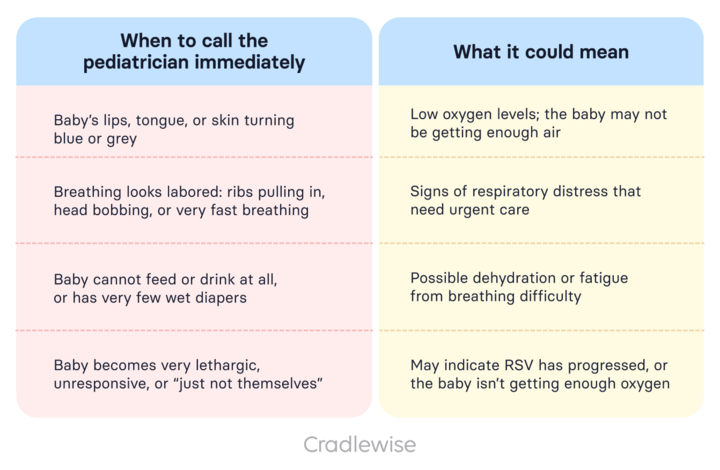
Note: These signs could mean the virus has moved into the lower airways (like bronchiolitis or pneumonia) and needs immediate medical attention.
Symptoms of RSV in babies
Symptoms refer to what your baby may be feeling on the inside — things you notice through changes in mood, appetite, sleep, or how active they seem. These patterns can help you understand when your baby is starting to feel unwell.
According to the CDC, these are some of the classic symptoms of RSV in babies:
- A runny nose, sneezing, mild fever (though baby might not have a fever, interestingly).
- A cough that starts mild but may deepen or become wheezy as the lower airways become involved.
- Fussiness, irritability: baby might be more clingy, awake more often at night because of breathing discomfort.
- Poor feeding or refusing feeds (because baby is too congested or tired to feed).
- In older infants/toddlers, you may see more “typical” cold symptoms (sore throat type behaviour, general malaise) but in babies under 6 months, it can present quite differently (even without a fever).
And remember, what starts looking like a “common cold” can shift from Bronchiolitis (inflammation of the small airways) or pneumonia in rare cases, especially in high-risk babies.
Jose Salas shares a clear rule of thumb for parents: “If your baby is struggling to breathe, not eating well, having fewer wet diapers, or seems extra sleepy, it’s time to call your doctor or go to the ER. When it comes to breathing problems, it’s always better to be cautious, it can be life-threatening.”
Why this can be trickier in newborns:
Since babies can’t tell you “I feel tight in my chest,” you must watch for changes in behaviour (less feeding, less playfulness), breathing patterns (that rib retraction, flaring nostrils), and overall alertness. If it seems “worse than expected for a cold,” trust your gut.

Did you know?
RSV is the leading cause of infant hospitalization in the U.S.
How long does RSV last in babies
When a baby is sick with a virus, parents often track every hour and day, hoping for signs of improvement. To make things easier, here’s a simple breakdown of what the RSV timeline usually looks like, from that first little sniffle to recovery.
- According to the American Academy of Pediatrics, RSV symptoms typically are at their worst on days 3–5 of illness.
- Symptoms generally last around 7–14 days in uncomplicated cases.
- That said, when the lower airways are involved (bronchiolitis, pneumonia) recovery can take longer: sometimes 2–3 weeks or more, with added breathing support or oxygen needed in hospital settings for high-risk babies.
A quick timeline guide for reference:
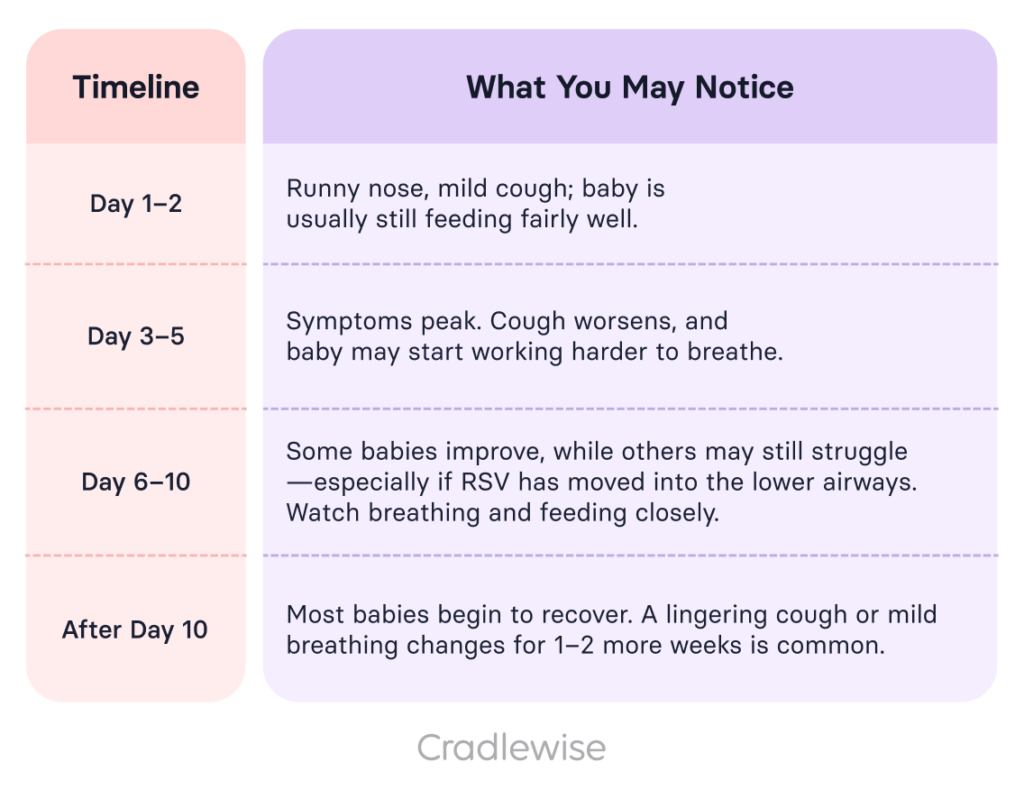
So if your little one is still coughing a bit two weeks after that first sniffle, don’t worry, that’s pretty normal.
Why this common virus can turn serious in newborns
Now here’s the “aha” part: RSV is common, but this is why it worries us more in babies:
- Immature lungs: Newborns, especially pre-term or under 6 months, have smaller airways, which means any swelling or mucus (like RSV can cause) takes up a bigger portion of that space and can hamper breathing much more quickly.
- Limited immunity: They haven’t developed strong immune defences yet, so even a “regular” virus can feel like a big deal.
- High risk of lower-airway involvement: With RSV the virus can move from upper airways (runny nose, cough) down into the small airways (bronchioles) and lungs, leading to bronchiolitis or pneumonia.
- Hospitalisation stats: For infants under 6 months, 2-3 out of every 100 may need hospitalisation when RSV hits.
- Risk factors make it worse: premature birth, chronic lung disease, congenital heart disease, and immunocompromised babies; all these increase the risk.
In short, what might be mild in a toddler or older child can become significantly more serious in your tiny baby because their system is still so delicate. That’s why we take this virus seriously, with love, not panic, but with care.
What to do as a parent?
While most babies will be fine with basic supportive care, the key is monitoring closely and acting early if things shift. Here are some practical tips:
- Keep the baby’s environment clean: minimize exposure to sick people, wash hands before feeding the baby, and avoid crowded indoor spaces if RSV is circulating locally.
- Monitor feeding and wet nappies: fewer feeds or fewer wet nappies = red flag.
- Observe breathing: is it harder? Are ribs or neck muscles moving more than usual? Nostrils flaring? That’s a signal.
- Comfort your baby: keep their nasal passages a bit clearer (use saline drops and gentle suction if needed), keep them upright during feeds if congestion is severe, and consider using a humidifier in the room (a cool-mist model can help).
- Stay in touch with your pediatrician, especially if your baby is experiencing feeding difficulties, breathing changes, or appears unusually sleepy. Better safe than sorry.
Immunizations to protect infants from severe RSV
The good news? There are now ways to help protect your baby from getting seriously sick with RSV. According to the CDC, parents can choose one of two preventive options, and most babies will only need one:
Table:
| Type of protection | Who it’s for | When it’s given | What it does |
| RSV vaccine (maternal) | Pregnant women | During pregnancy (usually in the third trimester) | Helps the mother pass protective antibodies to the baby before birth, offering early protection after delivery |
| RSV immunization (infant dose) | Infants and some older babies | Shortly after birth or at the start of RSV season | Gives babies direct antibodies to protect against severe RSV illness |
These tools don’t stop RSV entirely, but they significantly reduce the risk of severe infection, hospitalization, and breathing problems, especially in newborns, preemies, or babies with heart or lung conditions.
Talk to your pediatrician about which option is best for your baby, depending on when they’re born and the RSV season in your area.
Conclusion
Okay, you’ve done the reading, you’re tuned in, and that’s excellent. RSV in babies is one of those things that can feel like a chill cold, but because babies are so exquisitely vulnerable, the cold can escalate. However, remember that you’re not powerless. You’re the baby’s best monitor, their comfort, their safety net.
Watch the signs. Know the symptoms. And if something doesn’t feel right, don’t wait. Trust your gut. Your paediatrician is your partner in this.
FAQs
Q: What are the first signs of RSV in babies?
A: Early signs include a runny nose, mild cough, and reduced feeding. Watch for changes in breathing or alertness.
Q: How long does RSV last in babies?
A: RSV symptoms usually last 7–14 days, but a cough can linger for up to two weeks in some babies.
Q: When should I call the doctor for RSV?
A: Call right away if your baby has labored breathing, blue lips, refuses feeds, or seems unusually tired or unresponsive.
Q: Can RSV be prevented?
A: Yes. The CDC recommends either a maternal RSV vaccine during pregnancy or an infant immunization after birth
Q: Is RSV dangerous for all babies?
A: Most babies recover with home care, but it can be serious for newborns, preemies, or those with heart or lung conditions.
You may also like
- How do you prevent yourself from catching the flu while pregnant?
- Baby colic: How your newborn baby’s gut impacts their health
- Understanding the risk factors of SIDS and how to minimize them
Sources
- RSV in infants and young children: prevention and symptoms. Centers for Disease Control and Prevention (CDC). 2024. “RSV in Infants and Young Children”.
- When RSV is more than just a cold. HealthyChildren.org (American Academy of Pediatrics). 2024. “RSV: When It’s More Than Just a Cold”.
- AAP guidance on bronchiolitis in infants. HealthyChildren.org (American Academy of Pediatrics). 2023. “Bronchiolitis: When Your Child Has Trouble Breathing.”
- Understanding pneumonia and its connection to RSV. Centers for Disease Control and Prevention (CDC). 2024. “Pneumonia”.
You may also like



