Science of baby sleep
0 min read
What’s a healthy temperature for a newborn? A quick guide for parents

Cradlewise Staff
If you’ve just brought your newborn home, welcome to the magical (and mildly chaotic) fourth trimester. Your baby smells incredible, everything they do is adorable, and yet you suddenly have a million questions you didn’t think to ask at the hospital. One of the first big ones is: “Is my baby’s temperature normal?”
It’s the classic new-parent moment, you touch their little forehead, pause, and wonder if you should be worried. And because babies can’t tell us what’s going on, temperature questions pop up fast. You’re not alone. Every new parent has had this exact thought, and this quick guide is here to help you understand what’s normal, what’s not, and when to call your pediatrician. Think of it as that veteran-parent friend who shows up with coffee and answers.
What’s considered a normal temperature for a newborn?
Newborns run a little differently than we do, their temperature can shift more quickly, and they rely heavily on us to keep them comfortable. Newborns are still learning how to regulate their body temperature. Their internal thermostat (aka their thermoregulation system) is immature, so they can’t warm up or cool down as efficiently as adults. They also lose heat faster, up to four times faster, because their bodies have a higher surface-area-to-volume ratio and less insulating fat. And since they don’t have strong sweating or shivering abilities yet, even small changes in the room temperature or clothing can make a difference.
A typical healthy temperature range for babies hovers between 97–100.3°F (36–37.9°C) when using a digital thermometer.
The AAP says a rectal temperature of 100.4°F (38°C) or higher in a baby under 3 months is considered a fever, and that’s a “call your pediatrician right away” situation. Outside of that range, your baby might simply be adjusting to the room temperature, waking up from sleep, or getting a little bundled. Their temperature naturally fluctuates, totally normal!
What’s the best way to check my baby’s temperature?
Taking your baby’s temperature is one of those first-parent milestones that can feel a little intimidating, especially the first rectal check. The good news? You’ll get the hang of it faster than you think, and there are actually several types of thermometers you can use depending on your baby’s age and comfort level.
To make it simple, we’ve put together a quick guide comparing the most common digital thermometers, how they work, which ages they’re best for, and what parents need to know to get accurate readings.
Choosing the right thermometer for your baby
It’s normal to wonder which thermometer is best, how accurate each type is, and which one is safe for your little one.
According to the AAP, to not all thermometers are created equal, and the best choice depends on your baby’s age and how you plan to take their temperature. To make it easy, we’ve broken down the most common types of digital thermometers, how they work, the ages they’re recommended for, and the perks (and things to watch out for) so you can keep your baby safe and comfortable.
Check out the table below for a quick, at-a-glance guide to choosing the right thermometer for your newborn.

Why a digital rectal thermometer is best
The AAP recommends a digital rectal thermometer as the most accurate way to check a newborn’s temperature, especially for infants under 3 months. Rectal readings give you a true sense of your baby’s core temperature, which is critical in the early weeks when babies can’t communicate if something feels off.
If the idea of taking a rectal temperature makes you a little nervous, you’re not alone. Most parents initially feel that way. But with a calm moment and a little practice, it becomes much easier (truly!). Here are a few tips to help you get comfortable.
- Take the reading when your baby is calm
- Apply a tiny bit of petroleum jelly for easy insertion
- Only insert the tip (⅛–¼ inch)
- Keep one hand steady on your baby’s thighs
- Stick to rectal readings for consistency in the newborn stage
How do I know if my baby is too cold?
Newborns lose heat faster than older kids and adults. They’re small, their skin is thin, and they’re still figuring out how to regulate their body temp. Their internal “thermostat” is still developing, they lose heat up to four times faster than adults, and they don’t have much insulating fat, or strong shivering/sweating skills to help them warm up. That’s why the first few weeks are all about keeping them cozy, not overheated, just comfortably warm.
Signs your baby might be cold:
- Cool hands and feet (this is common, but check the chest or belly for a better sense)
- Pale or slightly mottled skin
- Sleepier than usual or slow to feed
- Feeling cool to touch on the torso
If you notice these signs, warming them up gently usually helps:
- Add a light layer
- Try skin-to-skin contact under a blanket
- Make sure the room isn’t drafty or overly cool
The CDC’s safe sleep guidance encourages keeping baby’s sleep environment comfortably cool and not using excess blankets. If your baby still feels cold after warming up or seems unusually sleepy or uninterested in feeding, it’s worth checking in with your doctor.
What if my baby feels too warm?
Overheating can sneak up on new parents, especially during those early weeks when we’re terrified our babies might get cold. But the truth is, newborns can become too warm just as easily, and that can also make them uncomfortable or irritable.
Common signs your baby may be too hot:
- Sweaty or damp hair
- Flushed cheeks
- Rapid breathing
- Hot chest or back (a better indicator than hands or feet)
- Fussiness or seeming “off”
If the warmth is coming from too many layers or a warm room, the solution is simple:
- Remove a layer
- Turn down the thermostat slightly
- Switch to a lighter sleep sack
- Make sure baby isn’t wearing a hat indoors, they trap more heat than you’d think
But, again if their rectal temperature hits 100.4°F (38°C) and they’re under 3 months old, the AAP says that counts as a fever and needs prompt medical attention.
How do I keep my home at a baby-friendly temperature?
Settling into life at home with a newborn means adjusting more than your sleep schedule, it often means adjusting the thermostat too. Babies are most comfortable in rooms set around 68–72°F (20–22°C).
Here’s a simple rule that works for most parents: Dress your newborn in one more layer than you’re wearing.
More tips for a comfy newborn environment:
- Opt for breathable fabrics like cotton
- Use a sleep sack for safer, more consistent warmth
- Keep baby dry, damp clothes or spit-ups cool them down quickly
- Avoid heavy blankets inside the crib
The CDC reminds parents that avoiding overheating is part of safe sleep. If you feel comfy in the room wearing a T-shirt, chances are your baby will too (with that one extra layer).
When should I call the doctor about my baby’s temperature?
Here’s the golden rule: If something feels off, trust your gut. You know your baby better than anyone, even in the first week.
Call your pediatrician right away if:
- Your baby is under 3 months old with a rectal temperature 100.4°F (38°C) or higher
- Your baby’s temperature is below 97°F (36°C) and doesn’t improve with warming
- They are unusually sleepy, hard to wake, breathing differently, or refusing feeds
- Their temperature fluctuates a lot and you can’t stabilize it
- You simply feel uneasy, and need another professional pair of eyes
Pediatricians expect these questions, and you’re never “overreacting” when it comes to newborns
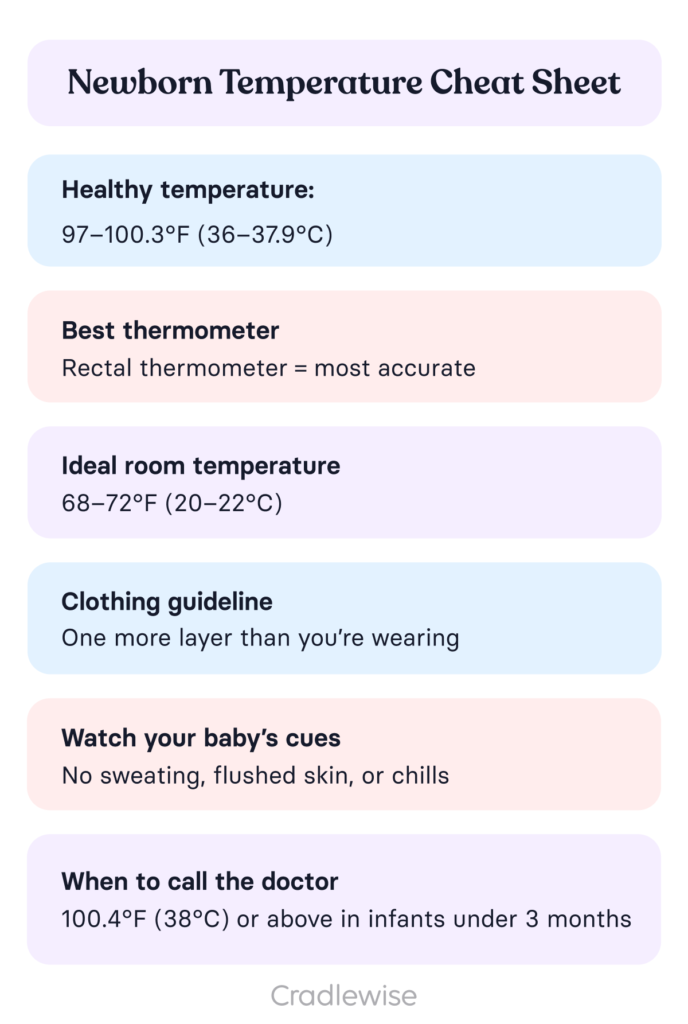
A quick, screenshot-friendly cheat sheet
Conclusion
Parenthood comes with a steep learning curve, and it’s totally normal to worry about whether your little one is too hot or too cold. The good news? You’ll get the hang of it faster than you think. Soon, you’ll instinctively know when to add a layer or let them breathe a little more.
For now, take a deep breath and give yourself some grace. Every tiny step counts, and the fact that you care this much already makes you an amazing parent.
FAQs
Q: 1. What’s the safest and most accurate way to check my baby’s temperature?
A: For babies under 3 years, a rectal digital thermometer gives the most reliable reading. It’s the method pediatricians trust because it measures your baby’s core temperature, not just the skin’s surface.
Q: 2. What’s considered a normal temperature for a newborn?
A: A rectal temperature of 100.4°F (38°C) or higher is considered a fever in babies under 3 months. At this age, even a small rise matters, so accurate measurement is key.
Q: 3. Can I use a forehead, ear, or underarm thermometer on my baby?
A: Forehead and ear thermometers can be helpful for older babies, but they’re not reliable for newborns. Underarm readings can be used as a quick check, but they’re often lower than the true temperature, so you’ll still want to confirm with a rectal reading if something feels off.
Q: 4. When should I check my baby’s temperature?
A: Take their temperature when they feel warmer than usual, seem unusually sleepy or irritable, refuse feeds, or just don’t seem like themselves. Your instincts count; if something feels off, it’s worth checking.
You may also like
- The ultimate guide to swaddling: Keeping your baby snug as a cocoon this winter
- Understanding the risk factors of SIDS and how to minimize them
- How sleep can boost the baby immune system
Sources:
- Guidance on fever in babies and when to seek medical care. HealthyChildren.org. 2025. “Fever and Your Baby.”
- Instructions for accurately taking a child’s temperature. HealthyChildren.org. 2025. “How to Take a Child’s Temperature.”
- Safe sleep guidelines for infants to reduce risk of SIDS. HealthyChildren.org. 2025. “A Parent’s Guide to Safe Sleep.”
- Brown adipose tissue in human infants. Handbook of Experimental Pharmacology. 2019. “Brown Adipose Tissue in Human Infants” pubmed.ncbi.nlm.nih.gov
You may also like



